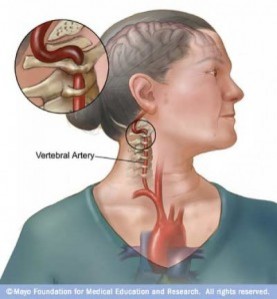
We now know from the works of many authors, but especially the case-crossover design work of Cassidy in 2008 and reflected again in 2017; that most likely a patient is arriving to your clinic with a stroke in progress. Briefly speaking, the practitioner must have felt the symptoms were musculoskeletal in nature, but instead, were of vascular nocioception and the headache/dizziness/etc was the symptom that led the individual to seek out help. Basically, a potentially fatal condition was missed. For us in the industry who keep up with this data, the trend is leaning towards a more global screening processes including the vascular system to make a more informed decision with positive results, but there are many cases that are still reported, including recently in a Family Practice Journal.
I recently stumbled upon two papers indicating a spontaneous dissection that led a patient to a healthcare provider—in these cases the treatment approach was not manipulation, but cupping and massage.
I can provide full texts to those who wish to read, but here is synopsis:
Choi et al 2016
We report an extremely rare case of spontaneous extracranial VA dissection presenting with posterior neck hematoma aggravated after cupping therapy.
“We presume that when spontaneous extracranial VAD occurred, his neck pain began and the cupping therapy caused a VA rupture and posterior neck hematoma with a pseudoaneurysm.”
Dutta et al 2018
We present an unusual case of vertebral artery dissection in a 30-year-old male patient following an episode of neck massage….The current case demonstrates the hazards associated with neck massage and the potential for good outcomes in these patients if timely intervention is provided.
For those of you who treat headaches, neck pain and dizziness; albeit very rare, you should always keep in mind potential cervical artery dysfunction. It could arise spontaneously or after a trauma, even trivial. Although we are still working in a diagnosis and area of uncertainty, I would suggest these two reports correlate with our trend that the actual procedure doesn’t cause the stroke—but instead, the acute arterial event was occurring spontaneously which led to a patient coming to you for help.
In the Optimal Sequence Algorithm of our Cervicogenic Dizziness Course, this is a hot topic and one that I take very seriously. Alongside my fellowship mentor, Dr. Brent Harper, we have designed what we both find to be the most up-to-date and sound reasoning to rule out spontaneous and mechanical vascular event. We strive to improve the order of your examination definitely makes a difference — which is one of the major flaws behind the vertebral-basilar insufficiency (VBI) test.
Even though I find our approach is quite sound, I want to end this post with the conclusion from Choi et al 2016 as it is a solid statement and a major take-home point:
The clinical diagnosis of VAD is not easy with acute-onset neck pain, especially young patients with no evidence of cervical trauma and disease. With undiagnosed VAD, traditional remedies such as cupping and chiropractic therapy to reduce pain can aggravate spontaneous dissection and worsen symptoms…..Early diagnosis of VAD could prevent symptom aggravation and permanent neurologic deficit.
You can learn more about the screening and treatment process of Cervicogenic Dizzinesss through Integrative Clinical Concepts, where the author and his wife, a Vestibular Specialist, teach a 2-day course. Pertinent to this blog post, the first day provides the most up-to-date evidence review from multiple disciplines to diagnose through the “Optimal Sequence Algorithm” to assist in ruling out disorders and ruling in cervical spine, including determining if single or double entity exists.
If you would like to host a course for your staff (either a vestibular, neuro, sports or ortho clinic), please do not hesitate to contact me at harrisonvaughanpt@gmail.com for prices and discounts.
Authors
Harrison N. Vaughan, PT, DPT, OCS, Dip. Osteopracic, FAAOMPT
Instructor: Cervicogenic Dizziness for Integrative Clinical Concepts
Danielle N. Vaughan, PT, DPT, Vestibular Specialist
Instructor: Cervicogenic Dizziness for Integrative Clinical Concepts













Post a Comment
Post a Comment