KINESIOPHOBIA IS OFTEN MENTIONED WHEN DISCUSSING PERSISTENT PAIN, BUT WHAT IS KINESIOPHOBIA? AND HOW IS IT RELEVANT TO PHYSIOTHERAPY?
Pain-related fear is proven to be a predictor of ongoing disability in those with persistent pain, and is more predictive than pain intensity or structural findings (Vlaeyen, Crombez, & Linton, 2016; Vlaeyen, Haazen, Schuerman, Kole-Snijders, & van Eek, 1995; Waddell, Newton, Henderson, Somerville, & Main, 1993).
This was first mentioned by Lethem and colleagues (1983), with the “fear-avoidance” model attempting to explain why some patients react more strongly to pain than others.
The Fear-Avoidance Model illustrates that when a painful event is believed to be threatening, it can create catastrophising thoughts that movement and activity will result in further pain and reinjury (Larsson, Ekvall Hansson, Sundquist, & Jakobsson, 2016). As this continues, this becomes avoidance behaviour, causing disability, deconditioning and depression, creating a vicious cycle of fear and perpetual pain (Larsson et al., 2016).

Fear Avoidance Model - Vlaeyen (2016)
Kinesiophobia was first coined by Miller and colleagues (1990), as an aspect of the fear-avoidance model. Kinesiophobia is ‘‘a condition in which a patient has an excessive, irrational and debilitating fear of physical movement and activity resulting from a feeling of vulnerability to painful injury or re-injury’’ (1990, p. 36). It is now defined as a fear of movement, due to the fear of re-injury (Lundberg, Larsson, Ostlund, & Styf, 2006; Vlaeyen et al., 1995), with individuals who are highly fear-avoidant believing pain to be a sign of bodily harm, and that any activity causing pain is dangerous and should be avoided (Hapidou et al., 2012).
RELEVANCE TO PHYSIOTHERAPY
GENDER DIFFERENCES
Persistent pain is becoming increasingly more common, with chronic low back pain and neck pain being the highest cause of disease burden in Australia (Hoy et al., 2014). As previously mentioned, kinesiophobia is a stronger predictor for persistent pain than pain severity or radiological findings.
So kinesiophobia is a predictor of pain becoming persistent…should we then screen every patient for kinesiophobia?
Are there patients who are predisposed to kinesiophobia, and therefore more likely for their pain to become persistent?
Persistent musculoskeletal pain is more prevalent in females, in both the general population and in those seeking treatment (Stubbs et al., 2010), with response to treatment differing between genders (Wijnhoven, de Vet, & Picavet, 2006). It is documented that females are more sensitive to pain, describe higher pain intensities and report widespread pain more often than males (Popescu, LeResche, Truelove, & Drangsholt, 2010). Females use more analgesia, and report depression rates twice as high as males (Munce & Stewart, 2007). However, males tend to display lower quality of life levels and generally score higher on kinesiophobia testing (Rovner et al., 2017). Rovner and colleagues (2017) conducted a study subjecting males and females to the same painful stimulus and reported the differences between genders. Surprisingly, both genders reported experiencing the same severity of pain, but males displayed higher kinesiophobia, disturbance of mood and lower activity levels, while females described stronger social support, pain acceptance and higher levels of activity.
Based on this, although females have a greater propensity to develop persistent pain, males appear more likely to display kinesiophobia, with females more likely to display depression. While it may not be necessary to screen every patient, it appears more relevant to screen males for kinesiophobia, while screening females for depression and anxiety (Rovner et al., 2017).
SURGICAL INTERVENTION
KINESIOPHOBIA IS A PIVOTAL PREDICTOR OF PERSISTENT LOW BACK PAIN, BUT IS THERE ANY DIFFERENCE BETWEEN THOSE WHO UNDERGO SURGICAL INTERVENTION AND THOSE WHO RECEIVE CONSERVATIVE MANAGEMENT?
Svensson and colleagues (2011) investigated kinesiophobia in patients following discectomy surgery. Patients completed questionnaires following surgical intervention, assessing kinesiophobia, quality of life, pain levels, disability, function and patient satisfaction. Almost half the patients recorded high scores on the Tampa Scale for Kinesiophobia (TSK), while all other data was comparable between groups (age, gender, location of herniation and place of birth) (Svensson et al., 2011). Those displaying high levels of kinesiophobia had poorer outcomes in all aspects measured, with greater disability, greater pain, more depression symptoms, lower self-efficacy and more catastrophising thoughts than those without kinesiophobia (Svensson et al., 2011). The follow-up questionnaires were completed 10 - 34 months post-surgery, yet still had almost 50% of individuals displaying kinesiophobia (Svensson et al., 2011).
Patients with kinesiophobia tend to have more depression, with pain being closely linked to depression. The study found more than 50% of those who described anxiety or depression pre-surgery felt the same post-surgery (Jansson, Nemeth, Granath, Jonsson, & Blomqvist, 2005; Silverplats et al., 2011). Depression also appears to independently predict poor outcomes post-surgery (Svensson et al., 2011). Since kinesiophobia can be a cause of depression, based on Vlaeyen’s fear-avoidance model (Vlaeyen & Linton, 2012), preventing kinesiophobia may reduce depression symptoms.
It appears imperative that all patients be screened for kinesiophobia following discectomy. Given almost half the participants displayed kinesiophobia, it seems almost every second patient will display fear avoidance. If their kinesiophobia is not addressed, it is expected they will suffer higher pain levels, have greater disability and lower quality of life.
Fortunately, a study by Sullivan and others (2009) showed addressing psychological factors pre-surgery improved post-surgical disability and pain levels. While this study only investigated knee surgery, it appears relevant to extrapolate the data to low back pain.
By routinely screening individuals for depression and kinesiophobia, before and after lumbar surgery, and addressing those who display high levels of depression and kinesiophobia, physiotherapists should be able to reduce pain levels and disability following lumbar discectomy surgery.
ASSESSMENT
TAMPA SCALE FOR KINESIOPHOBIA
The Tampa Scale for Kinesiophobia (TSK) was designed by Miller and colleagues in 1991, in an attempt to quantify the extent of kinesiophobia in individuals.
The questionnaire has 17 questions, with a short form of 11 also available.
The full form is shown below, with the patient circling the number that most applies to each statement. The therapist must then invert the scores of question 4, 8, 12 and 16, for example if the patient scores 1 on question 4, this must be counted as a score of 4. Or if a patient scores 2 on question 8, this must be scored as 3. If these scores are not inverted, the total score will be quite different.
The therapist, after inverting the scores of questions 4, 8, 12 and 16, counts up the total score.

Tampa Scale for Kinesiophobia
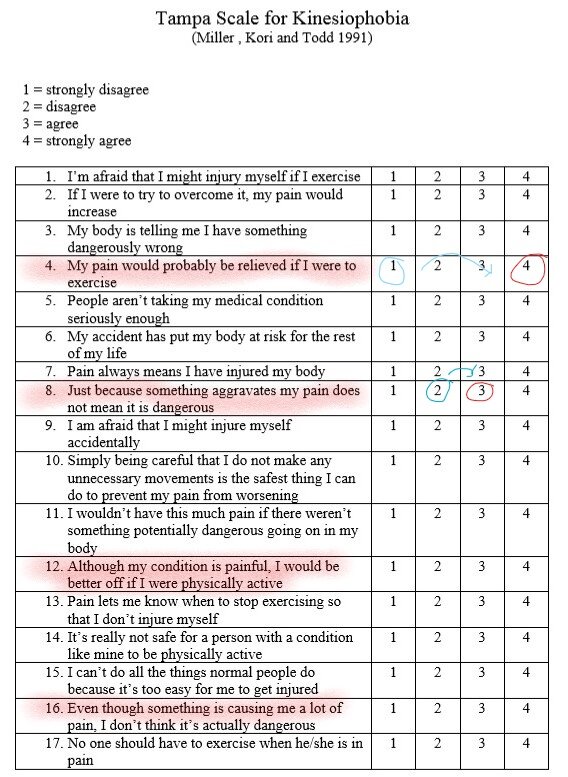
Tampa Scale with inverted scores highlighted.
There is no clear consensus regarding cut-off scores for high and low kinesiophobia. However, most agree a score greater than 37 shows high levels of kinesiophobia (Vlaeyen et al., 2016).
There also appears to be differences in gender, regarding cut-off scores. Branstrom and associates (2008) compared genders and found women with high TSK scores were younger than those with low scores. They also had more severe pain and higher disability.
Interestingly, a large proportion of males with persistent pain had a high TSK score (>37), yet there wasn’t a clear correlation with disability (Branstrom & Fahlstrom, 2008). The Rovner article (discussed earlier) had an average female age of 45, so perhaps didn’t pick up the subgroup of young females, who displayed more alarming pain, disability and kinesiophobia.
The authors suggest that differences occur between genders, and suggest using different cut-off scores, with perhaps a slightly lower cut-off for young females. This group of young females who scored highly on TSK had greater negative consequences, more severe pain and greater disability, so perhaps a cut-off score of 33 is more appropriate in identifying at-risk young females (Branstrom & Fahlstrom, 2008).
Kinesiophobia is a crucial aspect of persistent pain, with those scoring higher on TSK experiencing higher pain levels, greater disability and higher injury recurrence. The Tampa Scale for Kinesiophobia is a validated test, with a score of >37 being universally accepted as displaying high levels of kinesiophobia. It appears necessary to assess both young females, and males for kinesiophobia, with older females (>40) being at lower risk of experiencing kinesiophobia (Branstrom & Fahlstrom, 2008; Rovner et al., 2017). All patients following lumbar discectomy surgery should complete a routine TSK, to identify patients with kinesiophobia, at high risk of developing persistent pain.
Assessing and addressing kinesiophobia is crucial in managing those experiencing persistent pain, with a follow-up blog to come discussing management strategies.
Alicia Rayner - via Rayner and Smale
REFERENCES
Branstrom, H., & Fahlstrom, M. (2008). Kinesiophobia in patients with chronic musculoskeletal pain: differences between men and women. J Rehabil Med, 40(5), 375-380.
Hapidou, E. G., O'Brien, M. A., Pierrynowski, M. R., de Las Heras, E., Patel, M., & Patla, T. (2012). Fear and Avoidance of Movement in People with Chronic Pain: Psychometric Properties of the 11-Item Tampa Scale for Kinesiophobia (TSK-11). Physiother Can, 64(3), 235-241.
Hoy, D., March, L., Brooks, P., Blyth, F., Woolf, A., Bain, C., . . . Buchbinder, R. (2014). The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis, 73(6), 968-974.
Jansson, K. A., Nemeth, G., Granath, F., Jonsson, B., & Blomqvist, P. (2005). Health-related quality of life in patients before and after surgery for a herniated lumbar disc. J Bone Joint Surg Br, 87(7), 959-964.
Larsson, C., Ekvall Hansson, E., Sundquist, K., & Jakobsson, U. (2016). Kinesiophobia and its relation to pain characteristics and cognitive affective variables in older adults with chronic pain. BMC Geriatr, 16, 128.
Lethem, J., Slade, P. D., Troup, J. D., & Bentley, G. (1983). Outline of a Fear-Avoidance Model of exaggerated pain perception--I. Behav Res Ther, 21(4), 401-408.
Lundberg, M., Larsson, M., Ostlund, H., & Styf, J. (2006). Kinesiophobia among patients with musculoskeletal pain in primary healthcare. J Rehabil Med, 38(1), 37-43.
Miller, T. W., & Kraus, R. F. (1990). An overview of chronic pain. Hosp Community Psychiatry, 41(4),
433-440.
Munce, S. E., & Stewart, D. E. (2007). Gender differences in depression and chronic pain conditions in a national epidemiologic survey. Psychosomatics, 48(5), 394-399.
Popescu, A., LeResche, L., Truelove, E. L., & Drangsholt, M. T. (2010). Gender differences in pain modulation by diffuse noxious inhibitory controls: a systematic review. Pain, 150(2),
309-318.
Rovner, G. S., Sunnerhagen, K. S., Bjorkdahl, A., Gerdle, B., Borsbo, B., Johansson, F., & Gillanders, D. (2017). Chronic pain and sex-differences; women accept and move, while men feel blue. PLoS One, 12(4), e0175737.
Silverplats, K., Lind, B., Zoega, B., Halldin, K., Gellerstedt, M., Rutberg, L., & Brisby, H. (2011). Health-related quality of life in patients with surgically treated lumbar disc herniation: 2- and 7-year follow-up of 117 patients. Acta Orthop, 82(2), 198-203.
Stubbs, D., Krebs, E., Bair, M., Damush, T., Wu, J., Sutherland, J., & Kroenke, K. (2010). Sex Differences in Pain and Pain-Related Disability among Primary Care Patients with Chronic Musculoskeletal Pain. Pain Med, 11(2), 232-239.
Sullivan, M., Tanzer, M., Stanish, W., Fallaha, M., Keefe, F. J., Simmonds, M., & Dunbar, M. (2009). Psychological determinants of problematic outcomes following Total Knee Arthroplasty. Pain, 143(1-2), 123-129.
Svensson, G. L., Lundberg, M., Ostgaard, H. C., & Wendt, G. K. (2011). High degree of kinesiophobia after lumbar disc herniation surgery: a cross-sectional study of 84 patients. Acta Orthop, 82(6), 732-736.
Vlaeyen, J. W., Crombez, G., & Linton, S. J. (2016). The fear-avoidance model of pain. Pain, 157(8), 1588-1589.
Vlaeyen, J. W., Haazen, I. W., Schuerman, J. A., Kole-Snijders, A. M., & van Eek, H. (1995). Behavioural rehabilitation of chronic low back pain: comparison of an operant treatment, an operant-cognitive treatment and an operant-respondent treatment. Br J Clin Psychol, 34(1), 95-118. Vlaeyen, J. W., & Linton, S. J. (2012). Fear-avoidance model of chronic musculoskeletal pain: 12 years on. Pain, 153(6), 1144-1147.
Waddell, G., Newton, M., Henderson, I., Somerville, D., & Main, C. J. (1993). A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain, 52(2), 157-168.
Wijnhoven, H. A., de Vet, H. C., & Picavet, H. S. (2006). Explaining sex differences in chronic musculoskeletal pain in a general population. Pain, 124(1-2), 158-166.
- NEW - Online Discussion Group
- Live cases
- webinars
- lecture
- Live Q&A
- over 600 videos - hundreds of techniques and more!
- Check out MMT Insiders














Post a Comment
Post a Comment