Abnormal cervical range of motion (ROM) has been used as part of the clinical decision making for the diagnosis of Cervicogenic Dizziness. The limitation in range of motion, as well as pain to palpation to upper cervical spinal structures, can help the clinician differentiate between dizziness of vestibular origin vs cervical origin.
I am classically more of an “eye-ball” kind of ROM guy but continuing to look for objective ways to assess cervical dysfunction to not only prove a difference to the patient, but also for goal setting.
Currently the gold standard and most objective way to clinically measure the ROM is the CROM device (Cervical Range of Movement). I was part of a study about a decade ago and used the device, but it is expensive (upwards to $400) and potentially necessary in a clinical environment. Plus — its ugly and patients feel weird with it on! I mean — she doesn’t look too happy does she 🙂

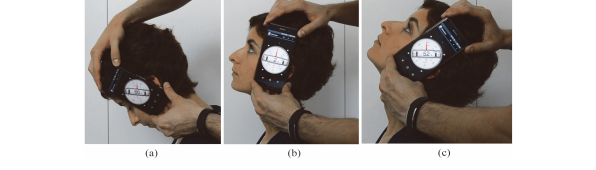
Cervical ROM is common in clinical assessment to examine individuals with pain. Nothing has really changed in the procedure for decades. However, the use of smartphone applications to measure ROM is gaining popularity. Considering majority, if not all, therapists have the phone handy throughout a session, it is time to utilize the technology.
I have found that patients perceive the phone technology as a higher value in clinical assessment, which could potentially place higher value on your overall treatments. This is anecdotal evidence but also seeing this more with applications to assess posture, running mechanics, etc that is more feasible in clinical practice vs laboratory settings. However, even with higher perceived value, we need to make sure the technology holds up to our gold standard—the CROM.
**Back story—I was part of an initial project about 10 years ago comparing different applications in a ceased website—therefore, have had the interest in other ways to measure ROM for years. The evidence out now of reliability and validity was not available back then**
A recent study by Rodriguez-Sanz et al 2018 examined two smartphone applications (Clinometer & Compass) against CROM for individuals with chronic pain and found:

- Excellent validity (>0.75) of lower and upper cervical spine movements
- Excellent intra-rater reliability (>0.75) of lower cervical spine movements
- Excellent inter-rater reliability (>0.75) of lower cervical spine movements
- Excellent intra- and inter-rater reliability of upper cervical spine extension movements
- Good intra-rater reliability (0.65-0.75) of upper cervical spine flexion movements
In conclusion, the Smartphone applications “Clinometer” and “Compass” have been proved of an excellent validity, by using CROM as gold standard in the lower cervical spine and upper cervical spine ROM measurements in subjects with 441 chronic cervical pain.
Based off of this study alone, I would feel confident as a clinician to use these applications to measure cervical AROM of the upper and lower cervical spine and knowing it will have solid validity and reliability against our gold standard, the CROM device.
Granted, the patients in this study were considered to have “chronic cervical pain”— which meant over the age of 18 and pain in cervical region for > 3 months. This hasn’t been studied specifically with patients with Cervicogenic Dizziness, but could be highly relevant as these patients have limitations in cervical ROM, especially cervical extension and rotation.
Now rock on smart phones!
Rock on more to save $400 for purchasing a CROM device in your clinic!
You can learn more about the screening and treatment process of Cervicogenic Dizzinesss through Integrative Clinical Concepts, where the author and his wife, a Vestibular Specialist, teach a 2-day course. Pertinent to this blog post, the first day provides the most up-to-date evidence review from multiple disciplines to diagnose through the “Optimal Sequence Algorithm” to assist in ruling out disorders and ruling in cervical spine, including determining if single or double entity exists.
If you would like to host a course for your staff (either a vestibular, neuro, sports or ortho clinic), please do not hesitate to contact me at harrisonvaughanpt@gmail.com for prices and discounts.
Authors
Harrison N. Vaughan, PT, DPT, OCS, Dip. Osteopracic, FAAOMPT
Instructor: Cervicogenic Dizziness for Integrative Clinical Concepts
Danielle N. Vaughan, PT, DPT, Vestibular Specialist
Instructor: Cervicogenic Dizziness for Integrative Clinical Concepts












Post a Comment
Post a Comment